Change of Life
The change of life is a term used to refer to the time in your life when you are no longer reproductively viable. For us women, that means we’re going through menopause.
That sounds like an awful thing. You hear about aging and missing hormones and everything kind of falling apart. But it doesn’t have to be that way.
The change of life can be an amazing chapter in your life.
Two things need to happen to make this chapter of your life the most amazing.
You need to be open to receive the blessings of the change. Because there’s a lot of blessings, more than grandbabies, much more.
As we Talk About Menopause We’ll Cover:
Menopause happens to all of us women eventually.
It’s happening to me right now. That’s right, me – the Hormone Queen® – going through the change. And it’s been a ten year transformational roller coaster ride.
It really helps to understand your hormones to be able to navigate the change. Especially your sex hormones – progesterone, estrogen, testosterone – the ones most affected by the change.
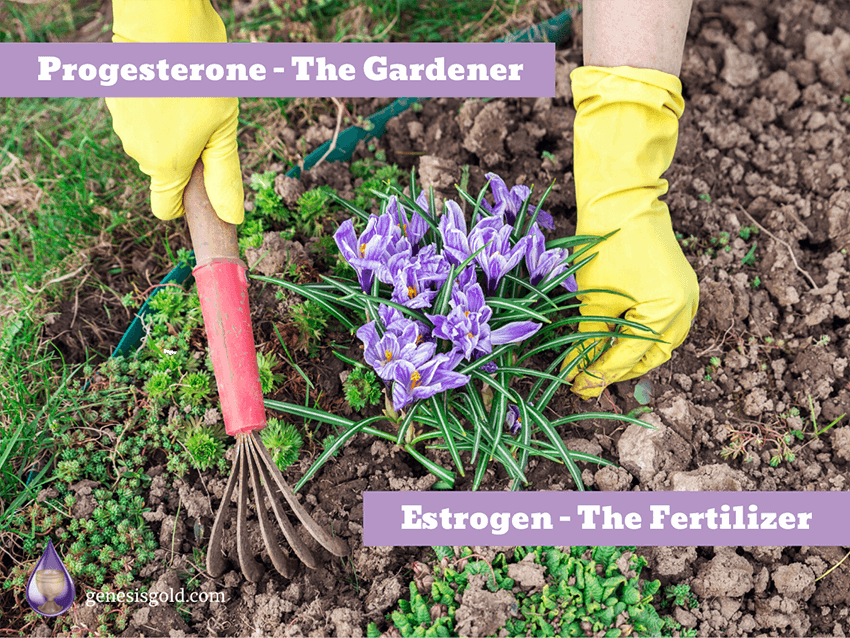
I like to call progesterone the gardener.
Progesterone keeps everything in check – knowing the difference between the flowers and the weeds. Progesterone supports healthy adrenal function and helps your brain make calming GABA.
Estrogen is the fertilizer.
It makes tissues lush, hair, skin, nails, vagina. Estrogen makes your brain hum with creativity. Estrogen promotes your sex drive. Estrogen makes everything grow, so it needs progesterone to help stop unwanted growth – like tumors.
Testosterone is the motivator.
It gives you your competitive edge. Testosterone also helps keep your bones and muscles strong.
Every woman is different in terms of how she responds to hormones
While in general progesterone is calming compared to estrogen, I know my brain really loves estrogen and my breasts get really sore with too much progesterone.
We’re all different.
Which is why I take a very individualized approach to assessing each of my female patients going through the change and developing a personalized healing plan that recognizes they are not like every other woman
For instance, the range of normal for estradiol is 40-400ng/dl – according to what time of your cycle that your blood levels are measured.
What kind of woman are you – hormonally speaking?
And the better question is what kind of woman were you when you were hormonally competent? Because your hormones probably were not measured then, when you were feeling great. So we have no baseline to compare to. Just some crazy new symptoms.
As an integrative nurse practitioner who’s helped thousands of women transition gracefully through the change, I hope to share my wisdom both clinically and personally with you.
So let’s talk about the change of life and how it affects you, and most importantly, what you can do about it.
What is the change of life?
The change of life is the time in a woman’s life when her hormones start to decline. After three decades of periods and fertility, your reproductive system begins to shut down.
You’re born with over a million ovum or eggs. By the time you reach puberty, you have about 600,000 left. And every menstrual cycle nearly 600 of those eggs try to be the egg of the month – but only one (and in rare cases two) will ovulate. The rest will die.
Most women have 12-13 periods a year. After 30-35 years, you run out of eggs.
No more eggs means no more sex hormones. And it’s the decline of your sex hormones – estrogen, progesterone, and testosterone – that cause all the symptoms of the change of life.
Your falling sex hormones cause a major disruption in the function of your hypothalamus.
Your hypothalamus is a small organ in your brain that controls everything.
Yes, everything.
All your hormones, your immune system, your neurological system, your digestion, your detoxification, your metabolism.
Your body temperature, your weight set point, your moods, your brain function, your sex drive, your energy, your stress response, your sleep, your rate of aging.
Everything.
When you go through the change, your hypothalamus has to adjust to your sex hormone decline. Without hypothalamic support, the adjustment phase can take years. Years of suffering from symptoms of sex hormone deficiency – which disrupts all your other hormones too – thyroid, adrenal, insulin, pituitary, pineal – and the rest of your body’s normal functioning.
TRANSFORM YOUR MENOPAUSE EXPERIENCE
When Do You Go Through the Change?
The change of life or menopause usually occurs on the average of fifty-one and a half years of age, but the range is much wider than that. It can start as early as 40. And as late as 60.
I get patients all the time asking me “When is this going to be over?”
Well, it helps to know where you are in the change of life.
The Three Phases of the Change of Life are:



– Phase One of the Change –
Perimenopause
Perimenopause is the 5-15 years before you finally have your last period. It’s characterized by inconsistent ovulation which leads to low progesterone and unopposed estrogen. Perimenopause is also known as pre-menopause.
Your periods become irregular. Your PMS intensifies. You should make 10-50 times more progesterone than estrogen, but you don’t if you’re not ovulating consistently. Estrogen dominance occurs when the two hormones are out of balance which causes water retention, bloating, and breast tenderness.
Your cholesterol rises because your liver is just trying to provide your ovaries with LDL cholesterol to make more hormones. The unused cholesterol and low progesterone triggers your liver to repackage sugar as fat which contributes to a thickening waistline.
Your imbalanced hormones affect your hypothalamus causing temperature intolerance and sleep disturbance. Your brain needs progesterone to produce calming GABA. As your progesterone plummets, you get moody and anxious.
What is the age range of perimenopause?
Most women will start perimenopause in their 40s.
If you stop your periods all together before you’re 40 years of age, and your follicle stimulating hormone (FSH) is elevated, and looks like you’re not fertile anymore – that’s called premature ovarian failure.
But if you stop your periods with an FSH over 30 after you’re 40 years old, it is considered menopause.
What are the symptoms of perimenopause?
Perimenopause symptoms can totally disrupt your life. And many doctors do not recognize your symptoms. So you can suffer for years until perimenopause ends when you haven’t had a period for at least 12 months. By then you’re in full blown menopause and you’ve aged rapidly.
If you recognize the symptoms of perimenopause early you can get the help you need.
If you’re having worse PMS – especially mood swings, increase in headaches, strange aches and pains that feel like you’re coming down with the flu – you may be starting perimenopause.
You may notice that you have more cramps. It kind of feels like you’re going through puberty again, like when you first started your periods. Perimenopause seems to magnify your PMS symptoms.
Breast tenderness can increase when you’re perimenopausal. That’s because your progesterone has lowered too, more so than estrogen. So your breasts can get uncomfortably full and tender. So much so that you can’t wait to take your bra off!
Irregular periods come with the territory. As you run out of eggs, you make less progesterone which is the hormone that regulates your periods. Now it’s true that a few women will have 28 day cycles right up to menopause and then stop, but they’re the rare ones. Most of us start having our periods closer together then skipping cycles for years before we have that final period.
I believe mood swings are the most life altering perimenopause symptom.
You may have had mood swings as part of your PMS, but now it’s all month long. You’re anxious, irritable, and depressed. You cry at the drop of a hat. Little things that you used to handle with ease seem insurmountable. Everyone gets on your nerves. And you may even lose it completely and fly into a rage. Afterwards you feel like crap having said and done things you would never do if you were in balance. What’s happening?
Well, your declining estrogen level affects your serotonin production. Serotonin helps control your moods. And your diminished progesterone production means you make less GABA so it’s hard to stay calm.
GENESIS GOLD®
The best menopausal supplements support your entire neuro-immune-endocrine system, meaning your entire hormonal system, focusing on the boss of your body – your hypothalamus.
How do you know for sure if you’re in perimenopause?
Well, assessing your hormones is more of an art than a science. But there is a blood test you can get that measures your follicle stimulating hormone (FSH) to see if you might be going through the change.
The best time to check your FSH to determine if you’re truly in perimenopause is the third to fifth day of your period. (Day one is the first day you bleed.) Between day three and five of your menstrual cycle is when FSH should be at its lowest in reflection to how much estrogen you made the month before.
The frustrating thing is how much FSH shifts from month to month during perimenopause. So checking your level one time doesn’t always show what’s really going on. By the time you see your health care provider to get the blood test ordered and get the test done at the appropriate time of the month – your FSH can be back down to normal.
Your FSH rises and falls in response to how much estrogen you make. So if your levels are lower, FSH is higher. If your estrogen level is high, your FSH is lower. It’s a negative feedback system.
Generally if your day 3-5 FSH is starting to elevate – over 15 to 25mIU/mL – you’re in the perimenopausal phase.
And since perimenopause can last anywhere from five to 15 years, that’s a long time to guess what’s happening…
Until you finally have that last period and you’re officially menopausal.
The Second Phase of the Change – Menopause
Menopause means your periods have stopped. Your FSH stays over 30 – your pituitary gland is screaming at your ovaries to make estrogen. But you’re out of eggs.
Menopause can happen any time from 40-60 years, averaging 51 ½ years of age. Most women will go through menopause between 45 and 55.
But every women is different
Menopause is characterized by low estrogen. Hot flashes and night sweats are signs of low estrogen affecting your hypothalamic thermostat.
While testosterone is often prescribed for women with low libido, it is actually low estrogen that lowers your sex drive, creates vaginal dryness and diminishes your orgasmic potential.
Estrogen controls bone cell turnover, so menopause triggers rapid bone loss. Your eyesight diminishes, your skin becomes itchy and you’re more sensitive to allergens.
Of course, your periods stopping is the most classic sign of going through menopause.
What are the symptoms of menopause?
While there are many symptoms related to the Change affecting nearly every system of your body – once you’re in menopause – these are the most classic symptoms.
Hot flashes are the classic sign of menopause. 75% of menopausal women have hot flashes. It feels like you’re heating up for no reason. Your face gets flushed. You’re peeling off clothes even in the dead of winter. Your hypothalamus controls your body’s thermostat and when your estrogen levels fall, your hypothalamus has a difficult time regulating your body.
Suddenly you can’t sleep through the night. Insomnia is a sure sign your estrogen levels are falling. Your hypothalamus controls your sleep cycles – how much melatonin and prolactin you make to go to sleep and stay asleep. When your estrogen levels fall starting in perimenopause, you may be tired enough to fall asleep but you wake up a few hours later. Supporting your hypothalamus is a safe and effective alternative to taking estrogen for menopausal insomnia.
If you’re not getting enough sleep of course you suffer from fatigue. But it’s more than that. Estrogen influences how sensitive you are to insulin. And as your estrogen levels fall in premenopause, you become more insulin resistant. Which means you can’t get enough glucose into your cells to make energy. So you’re tired all the time.
Brain fog. Your memory is just not very good. You forget why you walk into a room. It’s hard to focus. You can’t remember names or even common words. Your hypothalamus is the gateway for memory and when it becomes out of balance because your ovaries are no longer producing enough estrogen and progesterone, your brain is in a constant fog.
Sex isn’t like it used to be. First of all your vagina is drier. You don’t make enough lubrication fast enough so intercourse hurts. Second, your libido seems to have disappeared. What’s happening?
Well, your vagina needs adequate estrogen to stay healthy and lubricate normally when you’re sexually aroused. Most menopausal women will admit that their libido is flat. That’s because most women’s sexual libido is driven by estrogen. While during menopause, testosterone is higher in ratio to estrogen, it’s not enough to overcome the loss of our main female sex hormone.
Remember, all of these symptoms are treatable, and we’re going to talk about treatment in a little bit. But it’s good to know what you’re looking for while you’re going through the change.
The Last Phase of the Change – Postmenopause
You can be going through menopause for years before you finally have that last period. And once it’s been two years since the very last period, you are now entering the postmenopausal phase.
Your periods aren’t coming back unless of course you start taking hormone replacement therapy. Taking exogenous hormones – meaning not what you naturally make but taking them orally, through the skin, or as pellets – can actually wake up your uterus, start building up that lining, and start what looks like a period. Again, it’s really not a period. It’s more of a hormone withdrawal bleed. Kind of like what happens when you’re on the birth control pills.
The postmenopausal phase is basically for the rest of your life after your last period. And it’s a time when you’re not just progesterone deficient, like in perimenopause or estrogen deficient like in menopause, but you’re also testosterone deficient.
All three hormones are really low at this time.
What are the symptoms of postmenopause?
Low estrogen causes memory loss leading to senile dementia.
Low testosterone and low progesterone contribute to osteoporosis since these two hormones help build new bone.
Everything becomes drier and thinner without estrogen – your lips, your skin, your hair, your vulva. Sex may become painful. Without estrogen producing collagen to support your pelvic organs, you’re prone to bladder infections and may have stress incontinence – meaning you pee when you cough or sneeze.
Without adequate estrogen to program your immune system properly, your risk of inflammatory diseases like heart disease, arthritis, diabetes, and even cancer increases.
And you start to lose muscle mass, bone mass with more collagen loss, wrinkles, more sagging skin.
Usually by this time your sleep is better but not always. And your hot flashes have calmed down but not always.

How long does the change last?
It’s interesting that about 10 years after most women go through menopause, typically between their 60s to 70s, they may notice what feels like a second menopause. They’ve been without any menopausal symptoms – no real issues for years and all of a sudden they get hot flashes again.
What is that?
Well, your adrenal glands actually produce enough hormones to kind of sustain you after menopause. Not enough that you’re completely without symptoms, but enough to just sustain you.
In fact, in countries that have a lot less stress and have healthier adrenal function, like in the Mediterranean countries, women don’t age nearly as rapidly as we do here in the United States. And I think a lot of that is due to the fact that their stress levels are lower and they have healthier adrenals going into menopause.
It’s your adrenal glands that keep your hormone levels up in the first decade of menopause. Your adrenals convert pregnenolone to DHEA which then converts to testosterone and then into estrogen. Not nearly as much as your ovaries did before you started perimenopause. And unfortunately your adrenals can only make about 5% of the progesterone your body needs.
If you have healthy adrenal function going into the change, then these super glands can help keep some of your hormones in balance, so you’re not feeling too many symptoms. But eventually your adrenals start to poop out in your mid 60s or so. And you feel like you’re going through menopause all over again.
It’s actually what I like to call – adrenopause – your adrenals switch to low mode at that time.
Complete the Change of Life Checklist to find out where you are in the change of life.
Symptoms of the Change of Life
You may have just a few of the symptoms. Or you may have all of these symptoms. The symptoms of the change of life begin in perimenopause and extend through postmenopause.
And the list of symptoms is long:
Hypothalamic responses to the Change:
Digestive tract responses to the Change:
Dermatological and Connective tissue responses to the Change:
Nervous system responses to the Change:
- Hot flashes
- Insomnia
- Weight gain
- Mood swings
- Low sex drive
- Night sweats
- Irregular periods
- Fatigue
- Anxiety
- Memory lapses
- Difficulty concentrating
- Irritability
- Depression
- Panic disorder
- Allergies
- Vulnerability to infections
- Body odor
- Digestive problems
- Nausea
- Constipation
- Bloating
- Vaginal dryness
- Gum problems
- Loss of breast fullness
- Itchy skin
- Rashes
- Wrinkles
- Skin tags
- Brittle nails
- Hair loss
- Stress incontinence
- Osteoporosis
- Headaches
- Burning mouth
- Joint pain
- Breast soreness
- Electric shocks
- Muscle tension
- Tingling extremities
- Irregular heartbeat
- Dizzy spells
Hypothalamic responses to the Change:
- Hot flushes
- Insomnia
- Weight gain
- Mood swings
- Low sex drive
- Night sweats
- Irregular periods
- Fatigue
- Anxiety
- Memory lapses
- Difficulty concentrating
- Irritability
- Depression
- Panic disorder
- Allergies
- Vulnerability to infections
- Body odor
Digestive tract responses to the Change:
- Digestive problems
- Nausea
- Constipation
- Bloating
Dermatological and Connective tissue responses to the Change:
- Vaginal dryness
- Gum problems
- Loss of breast fullness
- Itchy skin
- Rashes
- Wrinkles
- Skin tags
- Brittle nails
- Hair loss
- Stress incontinence
- Osteoporosis
Nervous system responses to the Change:
- Headaches
- Burning mouth
- Joint pain
- Breast soreness
- Electric shocks
- Muscle tension
- Tingling extremities
- Irregular heartbeat
- Dizzy spells
Begin Your Menopause Healing Journey Today!
Let’s Focus on the Top Five Menopause Symptoms
#1 Top Symptom: Hot Flashes
Most women associate hot flashes with menopause. And hot flashes can make your life miserable. There’s no rhyme or reason to menopausal hot flashes. You can have hot flashes multiple times an hour. You can have them just occasionally.
Some women just feel kind of flushed and warm. Other women are flashing and sweating constantly like seven flashes an hour or more. When you wake you up in the middle of night and you’re sweating, it’s a form of hot flashes called – night sweats.
How do you know you’re having a hot flash?
You’ll feel a rush of heat, that’s sometimes accompanied by a flushing of your skin. Your skin feels very hot. You may feel as if you’re going to faint. Oftentimes you will start sweating. The sweat usually starts at your head and chest. If you look at yourself in the mirror, you may notice that your cheeks and your chest are getting red and flushed.
You feel extraordinarily hot compared to everyone else around you. Your sense of heat does not make sense to the environment. Everyone else may need sweaters and you’re peeling your clothes off.
A hot flash kind of comes in a wave and it feels like it starts in your chest and goes up your neck, your face, your head and then spreads throughout your body.
When do hot flashes begin?
Hot flashes can begin anywhere from perimenopause through menopause and into postmenopause. You can start having hot flashes in perimenopause, although that’s not as common because hot flashes are caused by low estrogen levels, and most perimenopausal women are plagued by low progesterone levels before their estrogen levels bottom out.
You can also have hot flashes into the postmenopause phase because your estrogen levels continue to stay low. And if your adrenal glands are not supporting you very well, they’re kind of stressed out or fatigued, you’re not going to have enough estrogen produced by your adrenals to help regulate your temperature.
How do you treat hot flashes?
The key to treating hot flashes is to balance your hypothalamus. I prefer to balance your hypothalamus with nutraceuticals. But you can temporarily balance your hypothalamus using hormone replacement therapy.
Because it’s lack of estrogen dysregulating your hypothalamus and causing the hot flashes, it’s important to be sure you’re getting enough estrogen. Now, we’re just going for symptom control, not a blood level. The amount of estrogen that you made as a young woman is very particular to you. And you may be low for you and still fall into the norm of estradiol levels in your blood. The goal is to use just enough estrogen to suppress hot flashes.
But you cannot use estrogen without using progesterone. Remember progesterone protects you from estrogen’s growth promoting effects – helping to keep tumors at bay
Typically, healthcare providers tend to prescribe a synthetic version of progesterone called a progestin to protect the uterine lining. Yet synthetic progestin is not natural progesterone. It has a lot of side effects -elevated LDL cholesterol, depression, and weight gain.
And most importantly progestin does not protect the rest of the tissues, including the breasts, the colon, the skin, the brain. I prescribe progesterone with estrogen even if you don’t have a uterus.
The safest most effective way to treat hot flashes is to balance your hypothalamus. The best way to balance your hypothalamus is with a nutraceutical designed to support your hypothalamus’ whole function, not just it’s temperature regulation. Otherwise you will always be chasing symptoms.
By high dosing with hormone replacement therapy, or taking single herbal treatments, your hypothalamus is not going to be well supported and you will always be having to add different herbs or other supplements to deal with the side effects.
I created Genesis Gold® in order to support the hypothalamus in all of its entire function, including temperature regulation, and it’s particularly effective at mitigating hot flashes.
Now, if your hot flashes are extreme, meaning you have more than a few an hour, then you’re going to want to take extra Sacred Seven® amino acids which are amino acids that are formulated specifically to balance the hypothalamus. These are plant based amino acids and while they’re in Genesis Gold®, taking extra Sacred Seven® for one to three months when you first begin hypothalamic balancing with Genesis Gold® can make a huge difference in mitigating your hot flashes very quickly and resetting your hormone balance and temperature regulation.
I prefer to use bioidentical hormone replacement therapy – BHRT– as bioidentical hormones are best tolerated by women and seem to be safer. I also never prescribe hormones orally – by mouth – as they must go through your liver, and over time will increase your risk of blood clots.

#2 Top Symptom – Insomnia
Besides hot flashes, insomnia is one of the most aggravating symptoms that any woman can suffer from. No one wants to be tossing and turning in the middle of the night, having trouble falling asleep and then waking up in the wee morning hours.
Even if you’re not having night sweats, waking up in the middle of the night and not being able to go back to sleep is common during menopause. It affects over 60% of women going through the change.
You know you’re experiencing menopausal insomnia when you wake up between 2-4am and you can’t fall back to sleep.
What causes menopausal insomnia?
Insomnia in menopause is also due to hypothalamic dysregulation. Your hypothalamus controls your day/night cycles.
Within your hypothalamus are nerves -called hypothalamic nuclei – that are innervated by your exposure to light.
These nerves literally tell your pineal gland to produce melatonin after dusk and stop making melatonin at dawn. The hypothalamic nuclei are incredibly sensitive to light waves.
Now it’s an interesting process – what happens at dusk. The pink light of dusk blocks the blue light of daytime which turns on melatonin production. And when the sun rises, melatonin drops and your hypothalamus produces dopamine which stimulates a cortisol surge so that you can start your day.
There’s two reasons for having insomnia during the change.
First, when your progesterone levels start to fall in perimenopause, you start to have trouble falling asleep. And that’s because progesterone helps you to produce GABA, which then allows your body and your mind to relax so that you can start to fall asleep.
And as you progress through perimenopause and you enter menopause, you start having trouble staying asleep. You tend to wake up in the wee morning hours, usually between two and four am. Not always because you’re having a horrible night sweat.
Second, you wake up in the middle of the night because your low levels of estrogen cause your hypothalamus to be dysregulated.
Remember your hypothalamus controls your circadian rhythm, so when it’s out of balance your adrenal glands are triggered to produce cortisol at the wrong time! You’re supposed to produce high levels of cortisol after dawn, peaking between 8am and 2pm. But instead you’re producing cortisol spikes in the middle of the night
And it’s cortisol that wakes you up. You’re anxious, your heart’s racing, you may have a hot flash, you cannot go back to sleep. Usually we wake up because we have to urinate, but the inability to fall back asleep is because your estrogen levels are low and your cortisol levels high at night, which dysregulates your hypothalamus.
So how do you treat insomnia?
Well, taking hormone replacement therapy definitely will help with insomnia. Bioidentical hormone replacement therapy is preferred – estrogen to keep you from waking up in the middle night and progesterone to help you fall asleep.
Remember if you take estrogen, you should be taking progesterone anyhow to protect your tissues from unwanted growth. And of course taken in a transdermal form – through the skin – rather than orally so you do not increase your risk of blood clots.
Now taking estrogen and progesterone when your ovaries are no longer producing them is fine and can be taken for as long as you need it. Every woman is different. So whether you take hormone replacement therapy or not is an individual decision. Treating women’s hormones should be personalized, not by a general protocol where everybody gets the same thing and the same amount.
Melatonin can also help you deal with insomnia temporarily. Taking melatonin all the time, like any hormone taken constantly without a break, will suppress your ability to make it.
But your pineal gland should be producing melatonin all of your life. Granted, you’re producing less as you get older. The elderly make much less melatonin, sleeping for much shorter periods of time than young people do. But if you’re taking high doses of melatonin, particularly, you’re going to suppress your pineal gland’s ability to make melatonin. And you will become dependent on melatonin and having to take increasingly higher doses in order to sleep.
Now if you’re having trouble falling asleep short acting melatonin can work. If you’re having trouble staying asleep you want a long acting sustained release melatonin. But the most effective way to reset your circadian rhythm and not be dependent on melatonin or hormone therapy is to support your hypothalamus.
Your hypothalamus controls your day night cycles. And if your day night cycles are off, because your hypothalamus is dysregulated by your low hormone levels during the change of life then you’re going to have trouble falling asleep and staying asleep.
So it is crucial that you support your hypothalamus.
When your hypothalamus functions optimally it’s going to help you reach the deepest level of sleep at night and feel rejuvenated in the morning.
I love how the phytonutrients in Genesis Gold® and amino acids in Sacred Seven® support your hypothalamus to reset your circadian rhythm and help you sleep through the night.
It’s so amazing to me how much that your hypothalamus controls: including your rate of aging, your temperature, weight setpoint, your metabolism and how your body functions in the daytime versus the nighttime.
GENESIS GOLD®
The best menopausal supplements support your entire neuro-immune-endocrine system, meaning your entire hormonal system, focusing on the boss of your body – your hypothalamus.

#3 Top Symptom – Weight Gain
Menopause weight gain is the weight that you gain between perimenopause and the postmenopause phase.
Menopause weight gain is caused by the dysregulation of your hypothalamus by your lower estrogen and progesterone levels.
Once you run out of eggs, you produce less progesterone and estrogen which drastically affects your metabolism. So, you don’t produce the same amount of energy as you did when you were younger. You then tend to store the extra calories you consume as fat – especially around your middle.
You also gain weight in menopause because of your lower levels of all growth promoting hormones including testosterone, DHEA and growth hormone. You have less lean body mass muscle and your bones become thin. The loss of muscle mass especially decreases your metabolic activity making you’re more prone to putting on body fat.
So how do you know if you have menopausal weight gain?
Well, first of all, it’s definitely going to be related to going through perimenopause or menopause. And despite the fact that you’re eating a healthy diet and you’re exercising regularly – doing all the things that you may have done earlier in your life to maintain your weight or lose weight in the past, now you have difficulty losing that weight.
Menopause weight can be all over your body. But the most significant change in how you’re gaining menopausal weight is that it’s mostly in your torso, from your armpits down to your hips. Some women notice some fat increase in their buttocks and thighs, but mainly a thickening of their waist. Your breasts may get larger as well.
The thickening of your waist is not just unsightly. It increases your risk of metabolic diseases like diabetes and heart disease. Part of the reason women gain midline weight gain in menopause is the same reason men tend to gain belly fat – unbound testosterone. When your estrogen levels fall in menopause, your testosterone becomes unbound and more active – leading to higher cholesterol levels, whiskers, and belly fat.
Menopause also affects your adrenal glands because starting in perimenopause you’re producing less progesterone. Your adrenals need progesterone to make adequate cortisol. Because your hypothalamus is so dysregulated by your falling sex hormones, your HPA axis – hypothalamic-pituitary-adrenal axis – is highly activated. And so you’re responding to stress in an exaggerated way, producing a lot more cortisol than you really need.
Cortisol’s job is to release stored sugar to fuel your fight or flight response. But if you don’t use that stored sugar to actually get away from danger, you’re going to store it in your belly fat. So it’s really important that you get your hypothalamus back in balance in order to maintain your weight.
How do you treat menopausal weight gain?
Getting your hormones back into balance can really help. Now it’s kind of controversial because some women will find that actually taking hormone replacement therapy can cause weight gain. That’s because most of the time it’s not prescribed in physiological doses meaning the kind of doses that your body really needs.
HRT is often under-dosed so you don’t get enough or overdosed so you get such high levels of estrogen and not enough progesterone that you end up having estrogen related weight gain. More full thighs, hips, bustline and water retention.
So it’s really important that your hormones are in a good balance for you. Now, what’s a good balance for you and what’s a good balance for another woman are two different things. Every body is different. Endomorphs are naturally thin. Ectomorphs tend to put on weight. Mesomorphs are more muscular and may put on weight at menopause if they don’t stay active.
Have you always had issues with a thicker waistline? Or do you tend to gain weight in your hips and thighs? Once you’re in menopause weight gain tends to favor extra belly fat.
What one woman needs hormone wise in terms of her body type can be vastly different than on other woman. So we’re not treating blood levels because we don’t know what’s optimal for you. Just what’s the norm for most women. The best way to tell if you’re getting enough estrogen for you is if your symptoms are improving.
If you’re on an adequate amount of hormone replacement therapy after a few months you should be balanced out – symptom wise. I prefer to prescribe BHRT – bio-identical hormone replacement therapy – because I believe it’s safer. I also prefer transdermal BHRT through the skin or sublingual BHRT – under the tongue, as a second choice. Never orally – by mouth- because you don’t want to increase your risk of blood clots. Using bio-identical hormone replacement therapy individually dosed for you can actually help to get your weight in better control.

And of course, exercise is key to losing menopause weight gain. The best exercise for the change is anything you like to do that gets your heart rate up (aerobic exercise) three times a week. That can be cycling, swimming, rowing, dancing, power walking, running, whatever – it’s your choice.
Plus one long slow distance to burn fat – working out at a lower heart rate but much longer at least 45 minutes to an hour or more, once or twice a week. And weight resistance exercise at least twice a week. Plus stretching on a daily basis.
Now the problem with exercise is that really intense exercise will raise your cortisol levels and that will increase your weight gain. So your menopausal exercise needs to be moderate.
My favorite aerobic exercise to lose body fat and keep in shape is a HIT routine. HIT stands for high intensity training. But this one is simple and easy to fit into your life. What it consists of is a five to seven minute warm up, then three 20 second bursts of speed with one to two minutes in between each speed interval, then a five to seven minute cool down. So it takes less than 20 minutes to do. Remember to do HIT three times a week.
Now that I’m menopausal, I like to do power walking using a hill as my sprint and just going as fast as I can for 20 seconds up the hill. Studies show that HIT can improve cardiovascular health, pulmonary health, decrease insulin resistance, increase insulin sensitivity, and help you lose weight.
Weight resistance is important to build muscle and bone that you tend to lose in menopause. You want more lean body mass in order to stay fit and trim. You can use your own body weight, doing calisthenics, or you can use actual weights. There’s lots of different things that you can do for weight resistance – like yoga and Pilates – a couple times a week.
And the long slow distance again is any activity you enjoy. You can bike, you’re probably not going to be swimming for more than an hour but you can combine swimming and surfing, anything that’s really going to keep you moving for at least an hour. You want your heart rate at less than 60% of your maximum to help burn fat. And you’ll be burning fat for 24 to 48 hours after doing a long, slow distance.
And don’t forget to stretch daily. Your menopausal joints will thank you.
Now, if you’re already exercising adequately for you, and you’re still not losing that menopause weight, you have to look at your diet.
Each body responds to different diets. You probably know the diet your body responds to best. If you’re like most women, you’ve got to limit your sugars and your starches in order to burn body fat. That’s because body fat is made up of stored sugar in the form of triglycerides which are actually three sugar molecules on a fat molecule.
Sugars and starches are high glycemic index foods meaning they raise your blood sugar quickly. I created an insulin resistance diet for my menopausal patients to lose body fat. My insulin resistant diet focuses on adequate protein, healthy fats, lots of vegetables and low glycemic carbohydrates. So this diet combined with exercise will help you lose that menopause weight.
If you’re still struggling, you may need stress reduction techniques. Why is that important? Well, if you get stressed out, you’re going to make more cortisol which is going to make your body store more fat. So learning how to reduce your stress is huge. I have a calm meditation that works really well to train your body to produce GABA so that you can naturally calm down and reduce your cortisol production. And all of this is included – my insulin resistant diet, my exercise routine, and my calm meditation – in my Hormone Reboot Training.
But the main way that my menopausal patients have been successful at losing weight and keeping the weight off is by balancing their hypothalamus.
And I know that I am constantly talking about your hypothalamus, but it’s because it’s the most important organ in your body.
Your hypothalamus controls everything, including your weight set point and your metabolism. Your hypothalamus controls your metabolism by controlling your thyroid hormone production.
Your hypothalamus also controls your hunger and satiety – when you feel full, when you’re hungry, and how much you actually eat.
Your hypothalamus controls your ideal weight set point. So if you try to lose weight too fast, you actually mess up your hypothalamus and it’ll bring you right back to your original weight.
So it’s really important that you work with your hypothalamus while you’re trying to lose weight. My most successful patients use hypothalamic support with Genesis Gold®, and sometimes extra Sacred Seven®, while they’re doing the insulin resistant diet and exercising and stress reduction techniques, and they’re able to lose that extra body fat and keep it off.
It takes time to reset your hypothalamus – at least three months. And it takes time to set new habits – at least 40 days. So you’ve got to be patient with yourself. You’re not going to see dramatic weight loss right away.
Usually the first bit of weight that you see lost is water weight. Losing five to eight pounds of water weight in the first week to 10 days is not unusual. But when you’re menopausal and hormonally deficient, you may not see even that much weight loss at first because your metabolism is so much slower.
We’re trying to increase your metabolism by supporting your hypothalamus. And we’re trying to increase your energy expenditure and your mitochondrial output – the mitochondria are little powerhouses in your cells that produce energy – by exercising. And we’re trying to burn that extra body fat by reducing the amount of high glycemic index carbohydrates that you’re eating.
With the right hypothalamic support, you can lose menopause weight gain.
#4 Top Symptom – Irritability/Mood Swings
Moodiness is when your moods – your level of happiness, irritability, anger – is excessive to the situation. Most women have experienced this sometime in their life, usually related to PMS.
Being a woman is like being on a hormone roller coaster. During our reproductive years, we may suddenly feel exceptionally sad, depressed, anxious, irritable. And just a day later, a week later, we feel completely different. Because we’re in a different part of our cycle.
But when you begin perimenopause, you’re going to start noticing that your moods are swinging more dramatically. For some women, it’s mostly a kind of sadness, an unusual depression, a lack of motivation. For a lot of women, it’s rageful irritability. And for some women, it’s a chronic, angsty anxiety.
So what is moodiness and what causes it?
Well, your hormones affect your brain chemistry.
Estrogen promotes serotonin production. Progesterone promotes GABA production. Testosterone promotes dopamine production. So when your hormones are out of balance, it affects the way your brain functions and it affects your moods.
Your hypothalamus is the gatekeeper for the neurotransmitters that control your moods.
And that’s because your moods are definitely related to your survival. You need to know when to be anxious and actually have a life saving stress response.
It’s your hypothalamus that instigates the bonding hormone oxytocin, produced between lovers, produced by mothers as they cuddle their newborns.
Your hypothalamus controls how we socialize, how we bond, how we interact with others and nature, by controlling our brain chemistry so that we can actually be safe and survive in this world.
And our hormones affect the production of our neurotransmitters. As our hormones decline during the change of life, those neurotransmitters are not produced in adequate amounts to keep our mood stable.
If you already have a mood disorder, depression, anxiety disorder, you’re bipolar. If you had postpartum depression, you’re more likely to have issues during perimenopause and menopause. It’s not unusual for your mood disorder to get worse because your hormones are depleted during the change.
How do you know if you’re experiencing menopause related moodiness?
That’s what happened to me. At the age of 49, I began perimenopause. Still had periods, no weight gain, felt great. Except my level of happiness plummeted. I was exceptionally irritable. And I couldn’t seem to shake my own moodiness. Still I didn’t realize how much I was struggling.
Until one day my husband sat me down, held my hand and asked – “if you were your own patient, wouldn’t you offer yourself some hormones.”
Taking Genesis Gold® put off my perimenopause for 5-7 years later than my younger sisters. And I didn’t go through actual menopause until I was 58 – two years later than my mother. Being a lifelong athlete, I didn’t have enough body fat for adequate estrogen reserve so I had to consider BHRT .
Treatment options for menopause moodiness
Hormone replacement therapy is your first treatment option not a bumping of your medications. Using hormones along with the medications you’re already taking is possible but talk with your healthcare provider.
Bioidentical hormone replacement therapy can help a lot in trying to get your moods in balance. But without balancing your hypothalamus, you will have to use more and more hormones to stay stable. And that’s not safe in the long run.
So it’s best to balance your hypothalamus whether you choose to use BHRT or not.
When your hypothalamus is functioning optimally, your moods are much more stable. You’re not nearly as anxious. You’re not nearly as depressed. And you don’t go into a rage. You’re responding effectively for whatever situation you’re facing. And that’s because your hypothalamus is not so dysregulated by your low hormonal levels.
If you combine hypothalamic balancing with bioidentical hormone replacement therapy, you can use a lot less hormones, and you’re going to be much more in balance. Or if you can’t take hormone replacement then balancing your hypothalamus is the key to stabilizing your moods.
So again, I love to use my Genesis Gold® for hypothalamic balancing. And the more severe cases, like those who have a history of postpartum depression or mood disorders, I’ll add some extra Sacred Seven® to their Genesis Gold® to give them extra hypothalamic support.
It’s just so important to keep your hypothalamus healthy and happy. It controls everything including your moods.

#5 Top Symptom: Low Libido or Low Sex Drive
Low libido basically means that you have a low sex drive. You no longer desire sex. You don’t think about it much. You may not have sex dreams.
A low libido doesn’t necessarily mean that you’re inorgasmic . You may still be able to orgasm. Although you may find that sexual arousal takes a lot longer.
If you’re like many menopausal women, you may have a low sex drive but also slow arousability and orgasm takes forever. And that’s because your hormones are out of balance.
What is low libido and what causes it?
When your estrogen levels fall, you’re not thinking about sex as much. Your partner doesn’t smell as enticing to you. You’re not finding their touch as enticing. In fact, estrogen helps your skin to stay stimulated. And when your levels fall, your erogenous zones are not as easily stimulated. It takes a lot more stimulus in order to feel aroused.
Low estrogen levels in menopause affect your blood flow. And less blood flow to your pelvic organs, to your clitoris, to your vagina, even to your uterus, makes sexual arousal much slower and orgasm take a lot longer.
You have less vagninal lubrication, making your vagina drier, and sex can be painful without artificial lubrication. I like to recommend natural lubricants like coconut oil, but it’s still not your lubricant and it’s still taking longer to orgasm.
Not that you don’t want to. It’s just harder to get over the hump. And that’s because you have less blood flow to your pelvic organs.
So how do you treat low libido?
Again bioidentical hormone replacement therapy can really help with treating low sex drive in menopausal women. And getting your vagina healthier with some estriol vaginal cream can make a huge difference in how responsive to sex play you are. Better vaginal lubrication makes sex much more comfortable. Sometimes that’s all that’s needed – estriol vaginal cream.
Now, I don’t necessarily use testosterone first to raise a menopausal woman’s sex drive. I know lots of healthcare providers love to prescribe testosterone for low libido but for the majority of women our libido is actually driven by estrogen, not testosterone.
So one way you can think of it is that a testosterone driven sex drive is the need to just orgasm. Not that women don’t have the need to just orgasm sometimes but testosterone is not the main driver of female sex drive.
Estrogen fuels our libido. Its estrogen that brings sensual enjoyment to sex. Estrogen drives our need for sensual foreplay, our need to be aroused, our need to be wined and dined. And that’s why your falling estrogen levels in menopause can flatten your libido.
Healthy estrogen levels fuels women’s sex drive.
So getting your estradiol levels up first with bioidentical hormone replacement therapy is the key to raising your sex drive. If that’s not working, and your FSH is is suppressed meaning it’s nice and low on estrogen therapy, and your vagina is healthy, and you’re not having hot flashes, you’re not insomniac, and you’re not moody, then you have enough estrogen on board so adding a little bit of testosterone may make a difference.
In my clinical practice, I’ve seen women treated with high doses of testosterone. And yeah, their sex drive goes up but they also get very irritable, very angry and grow whiskers that they don’t want.
So start with estrogen.
And remember you cannot take estrogen without progesterone, otherwise you’re not protecting tissues against the growth promoting effects of estrogen.
Again, I have found that in my patients who have a low sex drive that when they support their hypothalamus their libido returns. Because it’s your hypothalamus that controls your sex drive. It controls your reproduction rate, and your willingness and ability to be a sexual being. It controls your dreams and your sense of eroticism.
It’s vitally important to support your hypothalamus in order to have healthy sexual experiences like you enjoyed in your youth.
Now, a lot of menopausal women will find that they actually have a much better sex life during the change. And the reason is they’re no longer afraid of getting pregnant. And they’re more comfortable communicating their needs to their partner. And they’re at the point in their life where they’re not as concerned about how they look, they’re much more concerned about how they feel and they’re able to really surrender to their sexual experiences.
I find that my patients who use Genesis Gold® to support their hypothalamus are more likely to have this fuller experience, especially if they’ve had poor sexual experiences earlier in their life. Balancing their hypothalamus gives them a sense of empowerment over their sexuality.
My patients who support their hypothalamus with Genesis Gold® also find that their vagina stays juicier and their sex drive is healthy. The vast phytonutrients in Genesis Gold® helps increase hormone receptor site sensitivity so their declining estrogen levels are not such a problem.
TAKE CONTROL OF YOUR LIFE WITH MENOPAUSE
What are the best supplements for the change of life?

The best menopausal supplements support your entire neuro-immune-endocrine system, meaning your entire hormonal system, focusing on the boss of your body – your hypothalamus.
Herbal remedies may temporarily relieve symptoms but will not support your hypothalamus for optimal health from perimenopause through postmenopause.
The safest most effective way to treat the myriad of change of life symptoms is to balance your hypothalamus. I prefer using nutraceuticals. Taking single herbs like estrogenic black cohosh or androgenic maca or progestational chasteberry can help temporarily but over time will cause more imbalance in your hypothalamus.
The best way to balance your hypothalamus is with a nutraceutical designed to support your hypothalamus’ whole function, not just it’s temperature regulation, or it’s weight set point, or its circadian control. Otherwise you will always be chasing symptoms.
By high dosing with hormone replacement therapy, or taking single herbal treatments, your hypothalamus is not going to be well supported and you will always have to increase your dosage of hormones, or add different herbs or other supplements to deal with the side effects.
Your hypothalamus needs specific nutrients to do its job. Like a unique blend of specific amino acids formulated to support optimal hypothalamus function. And a rich array of phytonutrients from sea vegetation and sprouted whole plant foods to optimize hormone metabolism and function. A special herbal blend designed to increase your longevity and protect your cells. Plus phytonutrients to improve menopausal digestion and detoxification.
One Bag of Genesis Gold®
30-Day Supply
Subscribe and save 10%!
 Keeps Your Hormones in Harmony®, Balances Your Brain Chemistry and Optimizes Your Immune Function
Keeps Your Hormones in Harmony®, Balances Your Brain Chemistry and Optimizes Your Immune Function  Heals Your Hypothalamus with a special blend of plant based amino acids
Heals Your Hypothalamus with a special blend of plant based amino acids  Provides whole plant food micronutrients to optimize your digestion and detoxification
Provides whole plant food micronutrients to optimize your digestion and detoxification  Increases your energy by enhancing mitochondrial production
Increases your energy by enhancing mitochondrial production  Improves your sleep by normalizing your circadian rhythm
Improves your sleep by normalizing your circadian rhythm
Three Bags of Genesis Gold®
90 Day Supply
Save $50!
 Keeps Your Hormones in Harmony®, Balances Your Brain Chemistry and Optimizes Your Immune Function
Keeps Your Hormones in Harmony®, Balances Your Brain Chemistry and Optimizes Your Immune Function  Heals Your Hypothalamus with a special blend of plant based amino acids
Heals Your Hypothalamus with a special blend of plant based amino acids  Provides whole plant food micronutrients to optimize your digestion and detoxification
Provides whole plant food micronutrients to optimize your digestion and detoxification  Increases your energy by enhancing mitochondrial production
Increases your energy by enhancing mitochondrial production  Improves your sleep by normalizing your circadian rhythm
Improves your sleep by normalizing your circadian rhythm

Genesis Gold® provides your hypothalamus with exactly what it needs to start functioning optimally again:
Genesis Gold® provides phytonutrients to help your body fight off infection, decrease menopausal hypersensitivity and allergy reactions and suppress autoimmunity.
Genesis Gold® provides amino acids and phytonutrients to stabilize moods, deepen sleep, enhance memory, improve focus and concentration.
Frequently Asked Questions …
What age does menopause start?
The average age of menopause is 51 and a half years old. That’s when you have your last period. Perimenopause can start as early as 40. The entire change of life typically occurs between about 45 and 55 years of age. And for some women, up to 60 years of age.
When is menopause over?
Menopause is considered over when you have not had a period for at least two years. Going through menopause can last 2-15 years including the perimenopausal phase when your hormones begin to decline and you experience symptoms like hot flashes, brain fog, insomnia, weight gain, low libido. The average age of menopause is 51 ½ years old, but menopause can occur as early as 40 and as late as 60. Typically, women can expect to go through menopause about the same age their mother did.
When does menopause start?
Menopause starts when your sex hormones begin declining. For most women that’s between 45-55 years old, but can start as early as 40. You’ll know you’re starting the change when your periods start to become irregular and you start to have symptoms of low estrogen and low progesterone. Typically, hot flashes, insomnia, mood swings and brain fog.
Why does menopause cause hot flashes?
Menopause causes hot flashes because of withdrawal of sex steroids particularly estrogen. When estrogen starts to decline it dysregulates your hypothalamus. Your hypothalamus is the part of your brain that regulates many of your vital body functions including your temperature control. So when your hypothalamus becomes dysregulated, you will start having hot flashes and night sweats. Hot flashes are a vascular response- they’re your body’s way of trying to cool you down from a surge of internal heat.
Can menopause cause headaches?
Yes, for some women menopause can cause headaches. These headaches are usually vascular, like migraines. They are caused by the fluctuation of your hormones, particularly the withdrawal of estrogen during menopause can cause migraine headaches. Low estrogen levels contribute to vascular tension and water retention which can lead to muscle tension headaches.
Can menopause cause anxiety?
Yes, menopause can cause anxiety. As your progesterone levels start to fall in perimenopause, you start to make less GABA which is your calming neurotransmitter. With less GABA, you become anxious, irritable, you may even start to have panic attacks. You may notice that your anxiety begins with extended premenstrual irritability during the perimenopausal phase. Typically health care providers will treat menopausal anxiety with anti-anxiety medications, but balancing your hormones particularly progesterone and supporting your hypothalamus is the most successful way of dealing with menopausal anxiety.
Can menopause cause dizziness?
Yes, menopause can cause dizziness. Dizziness can occur because of imbalances in the inner ear – the cochlea. Menopausal dizziness is caused by some nerve irritation which is a function of low progesterone and by low estradiol which causes changes in fluid level of your cochlea affecting your balance.
How many years does menopause last?
Menopause can last as long as two years and up to 15 years. Perimenopause can begin as early as 40 and you may not have your last period until you’re 55 or older. Menopause is a long transition from high reproductive hormone levels that keep your body healthy to nearly nonexistent estrogen and progesterone levels which cause the symptoms of menopause and signs of aging.
Can menopause cause weight loss?
Yes, some menopausal women actually lose weight. When their hormones deplete, they start losing lean body mass – muscle and bone – pretty quickly. What you’ll see on the scale is a loss of pounds, but you may not look any thinner. In fact you’ve now become a skinny fat person, meaning that you have more body fat percentage and less lean body mass.
Can menopause cause hives?
Yes, menopause can cause hives. Hives are an exaggerated histamine reaction caused by the fluctuation of estrogen and progesterone starting in perimenopause. Menopausal women can also experience crawling itching skin sensation caused by a shift in cortisol because your HPA axis is out of balance because your sex steroids are low.
Can menopause cause acne?
Yes, menopause can cause acne. Menopausal acne is very similar to pubescent acne. It’s because testosterone levels in menopause are quite a bit higher than estrogen levels. Testosterone increases oil gland production which feeds acne vulgaris bacteria on your skin.
Can menopause cause constipation?
Yes, menopause can cause constipation. As your hormone levels fall your bowels become sluggish -less peristalsis or intestinal movement. Everything slow down, your digestion is poor and you have less hydration in the colon, which does not allow it to move the digested food and form feces appropriately.
Can menopause cause a fever?
While menopause doesn’t cause an actual fever, it can cause what feels like a fever – hot flashes. Menopausal women will feel like their skin is burning up, but their core temperature -usually taken orally or rectally – is actually low. Some women will have aggravated autoimmune conditions because of the menopausal hormonal changes, and may notice fevers, but it is not a common symptom.
Can menopause cause shortness of breath?
There’s no reason why menopause should cause shortness of breath, unless you’re having a panic attack. The declining hormone levels in menopause can contribute to anxiety which can make you feel short of breath. If you’re experiencing shortness of breath, and especially if it’s with exertion meaning while exercising, walking up stairs, walking briskly, you should be evaluated by your healthcare provider to check your cardiopulmonary status.
Can menopause cause weight gain?
Yes, it’s actually quite common for menopause to cause weight gain. Menopause causes weight gain because as the hormone levels drop, your mitochondria which produce energy become less metabolically active. You produce less energy but consume the same amount of calories which become stored as fat. There’s also some muscle loss in menopause, which contributes to a decline in your metabolism making you more prone to storing body fat. The imbalance between estrogen and progesterone during menopause can cause water retention and bloating too.
How many stages of menopause are there?
There are three stages of menopause – perimenopause, menopause, and postmenopause. The perimenopause stage begins when your sex hormones begin to decline between 40- 45. The menopause stage follows with further hormone decline, more symptoms, and no periods. Once you’ve had no menstrual periods for over two years, postmenopause stage begins.
Will menopause make you tired?
Yes, menopause can make you tired. Low estrogen levels reduce energy production by your mitochondria, making you feel tired. Plus low estrogen levels in menopause contribute to insomnia which leaves you with less daytime energy. During perimenopause, your ovaries make less progesterone which can contribute to low adrenal function causing tiredness, especially in the late afternoon.
Are menopause symptoms hereditary?
While it does seem that women tend to go through menopause about the same age as their mothers, their symptoms may be different. If your mother, grandmother and aunts seemed to suffer from extreme menopausal symptoms, you may experience a similar degree of symptoms. That’s because we tend to inherit similar patterns of hormone receptivity. If your mother tends towards water retention or mood swings, you may too. That being said, how you live your life compared to your female relatives makes a big difference in whether you suffer through menopause to the same degree as they did.
Will menopause cause high blood pressure?
While menopause really doesn’t cause high blood pressure, lower levels of estrogen and progesterone can change the elasticity of your blood vessels. When your arteries are less elastic, it makes your heart work harder to get blood flow to your body. If you’ve already developed arteriosclerosis from poor lifestyle – lack of activity, poor diet, high stress – then going through menopause can aggravate your already stiff arteries causing high blood pressure.
Are menopause symptoms permanent?
Most of the symptoms are not permanent. The common symptoms like hot flashes, night sweats, insomnia – usually go away over time. But it may take up to ten years if you don’t support your hypothalamus. Lower metabolism contributing to weight gain can be permanent if you don’t work to increase your metabolism through exercise, improved nutrition and hypothalamic support. The signs of aging that starts in menopause does not seem to shift.